Presentation
This male in his mid 50s presented to the ER, and had a diabetic foot infection. He had WBC 21, vital signs stable, had a chronic wound for several months that became infected. Here’s a photo of the bottom.


What do you see? In medical school and podiatry school, it’s normal at this stage of the work-up to request X-rays and an MRI to rule out osteomyelitis. Maybe if there’s concern about necrotizing fasciitis, we might calculate LRINEC score.
The workup: Read the clinical clues
The problem is that once we are in surgery and we are cutting, none of that information guides intra-operative surgical decision making. MRI and CT scans don’t tell us whether that edema is necrotic. I never pull up imaging in the middle of a case to tell me where to cut. It also definitely won’t tell us whether we incise or excise (incise meaning making a cut, excise meaning we cut out chunks of skin and soft tissue that we discard). Using photos and a quick confirmation looking at the wound during rounds or in the pre-operative holding area, I can decide what the surgical consent and plan will look like. I’ve stopped relying on imaging and focus on reading the foot for acute infections.
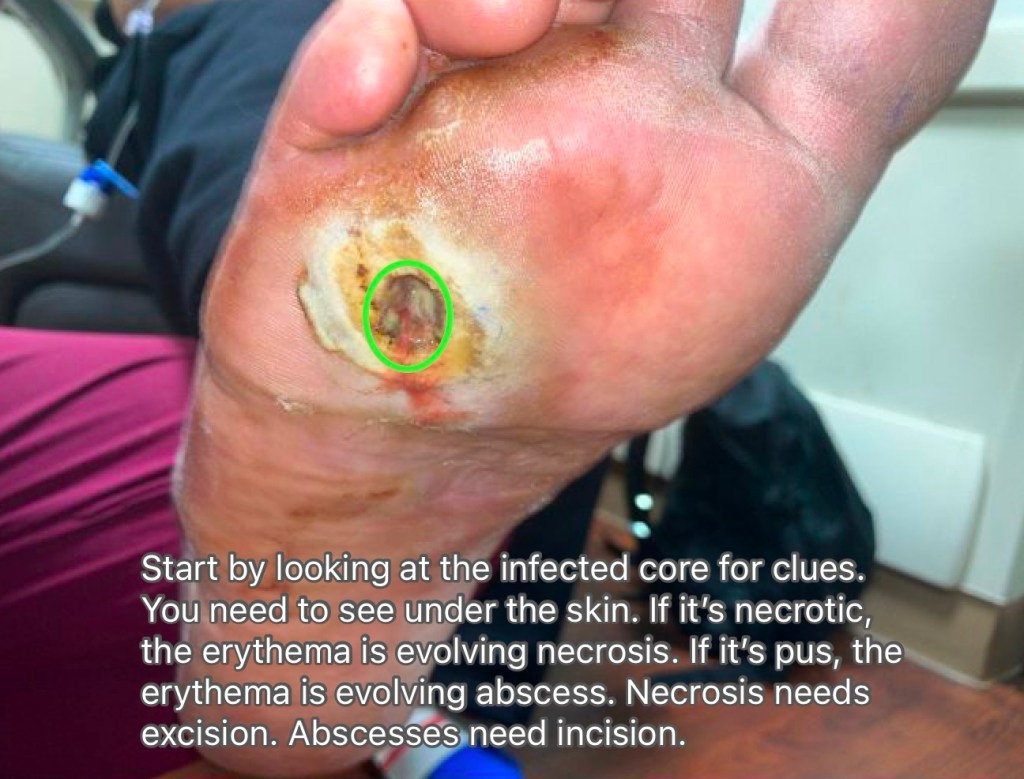
First, I look at the wound bed to see if it’s necrotizing or pus forming. If you zoom in closely, this wound bed appears to have a melted appearance of the deep tissues (liquefactive necrosis).

Next I look for blisters. It suggests internal bleeding due to exotoxins released by bacteria. Lastly, I take note of the edge of the erythema, which is evolving necrosis.
Consent Strategy

The blistered area is a big clue, it indicates end stage tissue death, the skin isn’t dead yet. Based on blister location, this needs at least a 4th ray amputation, probably a 5th ray. The erythema indicates evolving necrosis, we just don’t know how bad it is underneath, but I’m certain that the zone of necrosis is somewhere between the 4th ray, and the edge of erythma. So I have to be prepared to remove all of the erythematous skin. Patient needs to know he might not have any dorsal skin. Usually most patients don’t have a problem with a big wound, but losing toes can be difficult. In cases where I think ultimately they need a TMA, I’ll try to start with the minimum consent of a 4th ray with I&D. That gives them time to come to terms with losing more toes so I can get the consent for TMA at post-op rounds.

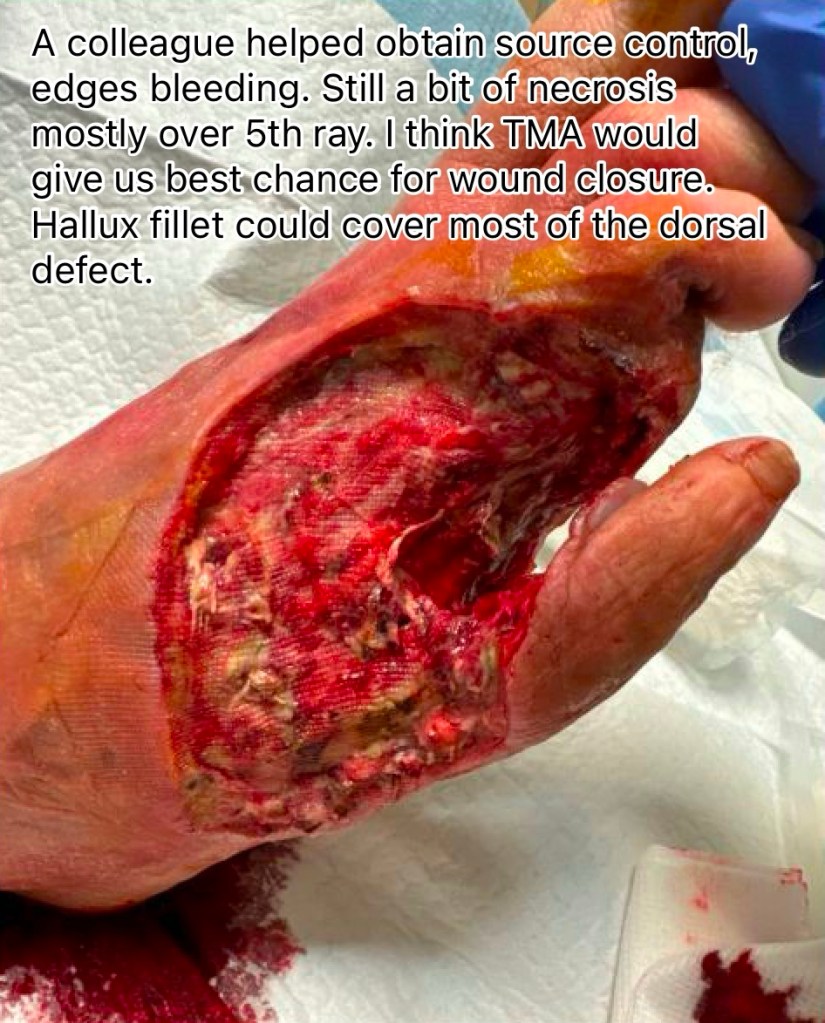
Notice that the damage to the 5th metatarsal was quite extensive. If we carefully now look back at the pre-op photos, I notice that the blister was indeed along that 5th metatarsal shaft. This is not by coincidence.

On post-op rounding, the skin edges look clean and granular. The EDL tendon stump looks a little goopy so it might need to be explored. The dorsal defect will heal fine and since it’s a NWB surface it won’t affect recovery all that much if we have to let it heal secondarily. Could also do a hallux fillet flap to cover dorsal. Mostly worried about the large 4th ray defect and 5th metatarsal bone exposed. The patient wanted to be healed as soon as possible, and so we planned for a TMA with hallux fillet flap to cover the dorsal defect.

How I closed this wound
During surgery I found a bit more pus along the extensor tendons, and so I opened two separate incisions along the dorsal foot to remove the tendons. Without toes, it’s better to be thorough with source control than to keep a non-essential tendon anyway. It looked beautifully clean after its removal. Then proceeded with the TMA incorporating hallux fillet flap. After the dissection was completed, I ran into a bit of a dilemma. I didn’t have enough skin to close over all of the bones, I had to pick either closing the 4th ray amputation site or the 5th metatarsal bone with the available skin.
However, while playing around with the skin flaps to see how they would close, I noticed that the abductor digiti minimi muscle was viable and had some bulk. So started to separate the muscle from the overlying skin, dissecting it just enough to be able to be flipped backwards to cover the 5th metatarsal bone. The plantar 5th metatarsal skin was then mobilized medial to cover the remaining defect. The rest was closed in layered fashion, 3-0 monocryl and 2-0 and 3-0 nylon.


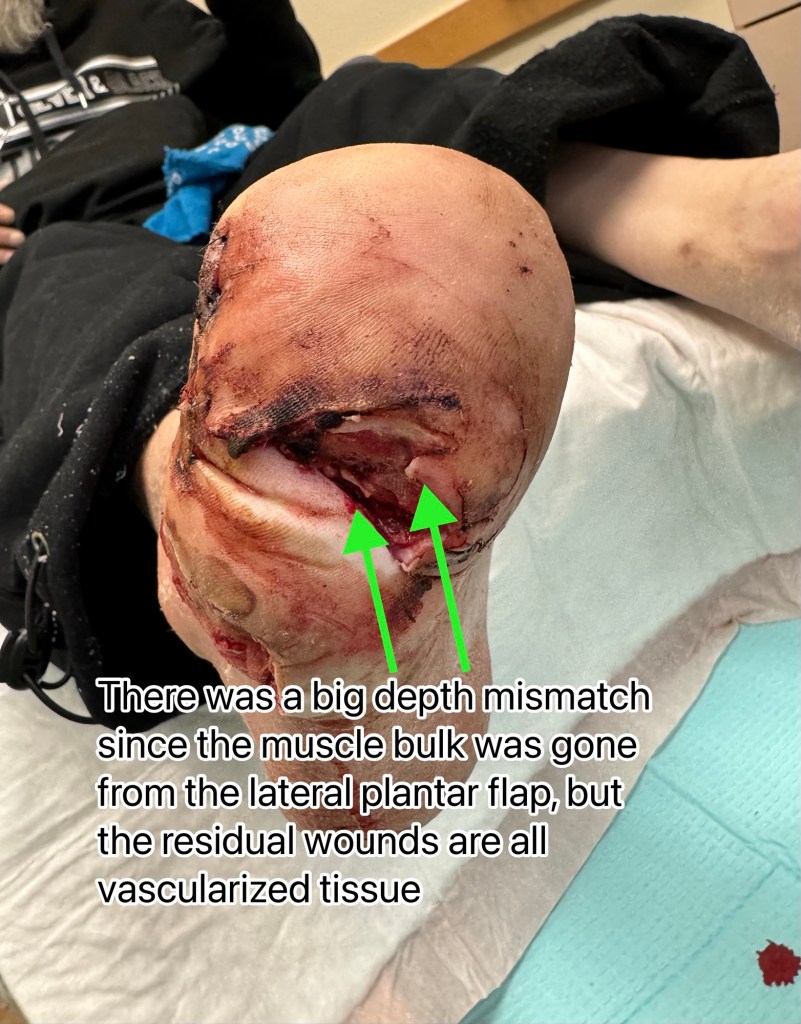
The medial plantar flap was stretched over laterally as much as possible, but due to repurposing the abductor digiti mini muscle, the lateral plantar flap had less bulk, creating a depth mismatch. However I’m not worried about that residual plantar wound, it’ll heal fine since we got all the bones covered. Same with the exploratory incisions, since there was a tiny bit of pus, decided to leave them open just incase. You’ll see this will heal just fine with minimal effort.
Here was the path report from the TMA.
DIAGNOSIS:
A. RIGHT FOOT:
– NECROTIZING SKIN ULCER WITH SUBJACENT ACUTE CELLULITIS/ABSCESS.
– SOFT TISSUE MARGIN POSITIVE FOR ACUTE CELLULITIS/ABSCESS.
– SKIN AND BONE RESECTION MARGINS ARE HISTOLOGICALLY VIABLE AND WITHOUT DIAGNOSTIC ABNORMALITY.
It confirmed type 1 necrotizing fasciitis with negative bone margins. He was discharged on oral Augmentin.
I see patients weekly after closure, with in-office debridement, betadine gauze dressings once a week. The fillet flap struggled a bit. Not much I can do at this point, just need to watch and let it demarcate.
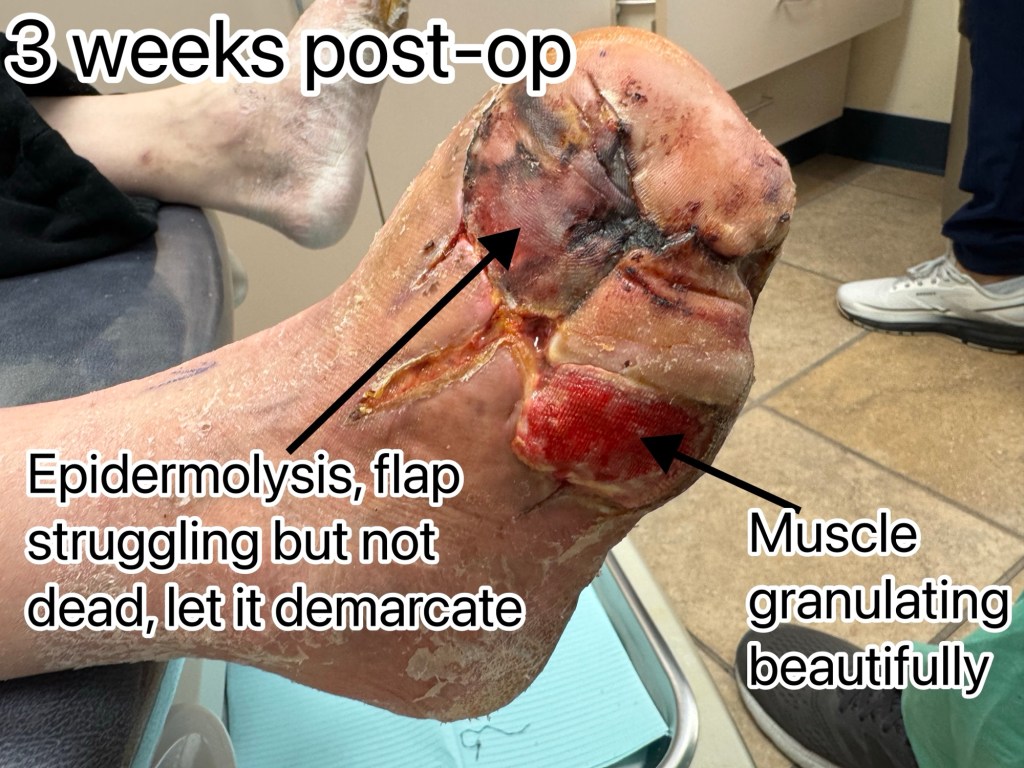










I’ll admit that prior to 2025, I was not comfortable doing muscle flaps, and I didn’t push myself to think that I needed to do it because I was able to get wounds with exposed bone to heal with corticotomies and scaffold grafts. However, the result is literally skin and bone… very difficult to sustain the test of time with patients needing to walk on that surface. It might be okay for a very low level ambulator, but for someone active like this patient, soft tissue bulk is needed over bone. Plus once I learned the dissection technique, it wasn’t technically very difficult to perform.
